When to Use FHIR vs. EDI in 2026: Decision Trees for CIOs and IT Directors

Healthcare payers are facing a pivotal crossroads in 2026. Our experience helping teams navigate EDI and modern integration requirements has shown just how challenging, and rewarding, this convergence of standards can be. CIOs and IT directors stare down both regulatory pressure and internal demand for digital transformation. So here, we share clear, experience-based decision trees to cut through the hype and help you build a practical roadmap.
The 2026 Compliance Crunch: Why Timing Is Critical
The CMS mandate for FHIR API access by July 4, 2026, is non-negotiable and has far-reaching consequences for payers. But that doesn’t mean EDI (with its persistent ties to X12 834, 837, and 835) is going anywhere. Our sector must operate both worlds in parallel, which creates significant operational strain.

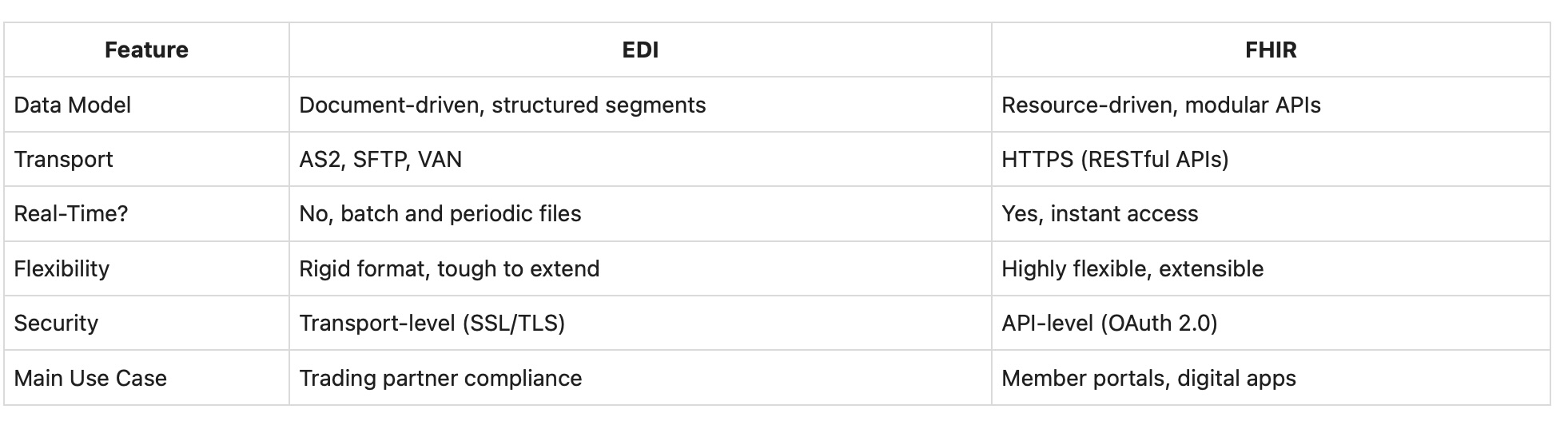
EDI vs. FHIR: What’s the Real Difference?
EDI: Rigid, Document-First Transactions
EDI is built on standard transaction sets: you transmit an entire enrollment file, claim, or eligibility record as one unit and expect your partner to process it as structured, batch-oriented data. Typical file types include:
- EDI 834 for enrollment
- EDI 837 for claims
- EDI 270/271 for eligibility inquiries and responses
- Positional, CSV, and XML files from non-standard sources
Transport is usually handled by secure connections like SFTP or AS2. EDI shines in regulatory workflows with established trading partners but can be inflexible if a source's file format shifts unexpectedly.
FHIR: Modern, API-Enabled Interoperability
FHIR, on the other hand, is built for modern web APIs. Data is modeled as discrete resources: Patient, Coverage, Claim, etc. It allows for:
- Real-time retrieval and updates (via REST APIs)
- Partial updates and granular access to specific fields
- JSON or XML payloads that are easier to work with for developers
- OAuth 2.0 and SMART on FHIR for secure, role-driven access
This model works best for interactive portals, mobile apps, and scenarios where users need just-in-time access to specific data.
Comparing EDI and FHIR
Decision Tree #1: Where Should You Start?
We've seen that your starting point comes down to your business priorities:
- Regulatory compliance and trading partner workflows come first? Invest in robust, multi-format EDI ingestion and validation. Ensure all files are standardized so you never fall out of compliance.
- Is member experience and digital transformation the priority? Begin planning for secure FHIR API enablement, focusing on those resources (Coverage, Claims, Enrollment) that will be most valuable to portals and mobile apps. Start small and iterate quickly.
- If you need both? (This is the common scenario.) Build a hybrid integration layer. Standardize all data as it enters your environment so downstream systems can consume it through either EDI routes or FHIR-enabled APIs depending on need.
Decision Tree #2: Tackling Multi-Format Enrollment Data
Realistically, payers rarely receive data in just one format. Manual mapping and validation is common, but it's not sustainable. We recommend moving to an automated standardization approach for these reasons:
- Manual mapping increases error rates and delays
- Files from different sources (employers, brokers, exchanges) often come in Excel, CSV, or XML, forcing your team to support each variation
- Compliance and audit trails are easier with a centralized, automated platform
Automating this layer lets your business scale and frees your technical resources to focus on high-value projects, rather than repetitive file cleaning.
Decision Tree #3: Building a Hybrid Integration Architecture
Hybrid is not just about technology, it’s about simplicity. By consolidating all inbound file variances (EDI, Excel, CSV, positional), we prevent operational surprises. Our clients generally take this phased approach:
- Stabilize EDI Operations: Clean, standardize, and validate all files immediately on arrival. Catch and fix errors early.
- Develop FHIR Strategy: Map which FHIR resources your business will need. Plan for secure API authentication and authorization with HIPAA and internal access in mind.
- Deploy Integration Platform: Let all data, regardless of source, pass through a normalization layer that logs transformations and supports both consumption paths: EDI flow or FHIR API.
- Expand Capabilities: Surface standardized data for real-time dashboards, member lookups, and analytics.
The Real Hidden Cost: Manual Processing Burdens
Our experience shows that IT teams often spend 25-50 hours a week on file validation and mapping before automation. Each enrollment or claims file that requires manual intervention is a drain on cost, morale, and speed. Automating the standardization process lets those teams focus on strategic projects, from FHIR API enablement to digital member engagement.
Realistic Example: Multi-Source Enrollment Intake
Picture this: Your largest group sends annual enrollments as Excel files. Brokers provide weekly CSVs. Some legacy employers still transmit EDI 834. Instead of different teams and tools for each, we recommend a single ingestion layer that detects format, normalizes the data, converts as needed for downstream EDI or real-time FHIR APIs, and logs all changes for compliance. This approach produces:
- Quicker, more accurate enrollment processing
- Reliable audit trails for compliance inspections
- Data immediately ready for internal member lookup or digital product experiences
We detail more about the value of data format standardization in this dedicated guide.
Key Roadmap Considerations for 2026
- Audit all inbound files and sources: This is foundational, because you can't improve what you can't see.
- Quantify manual workload: Estimate IT hours lost to EDI file mapping, validation, and troubleshooting.
- Identify quick FHIR wins: Prioritize member eligibility lookups or data access for top service teams.
- Define success metrics: Decide what quick resolution, compliance, and innovation mean for your business. For us, that’s typically measured in reduction of manual interventions, faster onboarding of new sources, or improved member portal capabilities.
What to Look For in a Hybrid Integration Platform
- Flexible Multi-Format Intake: True support for EDI, Excel, CSV, XML, and more using your real-world data, not just vendor demo files
- Real-Time Error Detection and Standardization: Files are validated, normalized, and failures are flagged for user-friendly review
- Security and Compliance Controls: Role-based access, complete audit trails, and encryption at rest and in transit, as described in our Trust Center
- Role-Friendly Usability: Business and IT staff should be able to check file status and troubleshoot issues without code
- Seamless Integration: Ensure the platform connects with your claims management, data warehouse, EDI translators, and supports both batch and API distribution
ROI: The Value for Different Stakeholders
- IT and EDI Teams: Reduction in manual support time and after-hours troubleshooting, so your talent can focus on new capabilities and improvement
- Customer Service and Operations: Instant access to clean data for member lookups, which previously relied on overnight batch processing
- Risk and Compliance: Proactive alerts and full transformation logs are key to passing HIPAA audits and meeting the 2026 FHIR mandate
- Business Intelligence: Real-time reporting and a single source of truth for analytics, eliminating the spreadsheet chaos that persists in many organizations
Practical Questions Before Investing
- How many formats hit your IT environment each month? (Do an internal file audit if you’re unsure.)
- How much time does your team spend manually processing enrollment and claims files?
- Which business cases could FHIR APIs unlock for you—member self-service, real-time eligibility, or faster claims tracking?
- Is your current integration layer ready for both regulatory deadlines and rapid business evolution?
Our Guidance for Healthcare Insurance CIOs and IT Directors
The coming year means critical choices for anyone overseeing payer technology. Most will need a hybrid approach: EDI for compliance with a robust, automated standardization platform, then FHIR to deliver modern member experiences and meet regulatory deadlines.
As you build this roadmap, our advice is simple: standardize first, automate where possible, and select a partner who can help you see and solve the entire integration puzzle, not just one transaction type.
Want strategic input on your roadmap? Our team at EDI Sumo has spent years unifying EDI and modern API operations for payers large and small. Learn more or reach out through our site at www.edisumo.com. We’re here to share best practices and help your team succeed in 2026 and beyond.


.png)






.png)

.png)


.png)
