Top Pain Points in Healthcare EDI Integration (and Proven Ways to Solve Them)


EDI (Electronic Data Interchange) is the backbone of automation for insurance payers, enabling seamless enrollment, eligibility, claims, and communication across the healthcare ecosystem. But after years of experience, we have learned that there is nothing “seamless” about healthcare EDI integration, at least not without solving some hard, persistent pain points first.
In this deep-dive, we’ll walk through the top EDI integration pain points we see repeatedly throughout the healthcare insurance industry, and more importantly, what practical strategies and solutions actually make a difference. We focus on the real-world issues that block operational excellence and frustrate IT, EDI, and enrollment teams year after year.
Why Healthcare EDI Integration Is So Painful
Healthcare EDI was supposed to bring automation, standardization, and transparency to enrollment, claims, and data exchange. But reality looks different:
- Siloed teams burning hours tracking files and reconciling exceptions
- Excel-based monitoring that creates blind spots and hidden costs
- Frequent disruptions that threaten SLAs and result in penalties
- IT teams drowning in manual exception handling, rarely finding time for optimization
- Compliance teams scrambling for audit trails and accuracy
If you’re in EDI, enrollments, claims, or IT at a health plan, you’ve probably seen these issues firsthand. Let’s break down these pain points in detail, then discuss proven ways successful payers are finally moving forward.
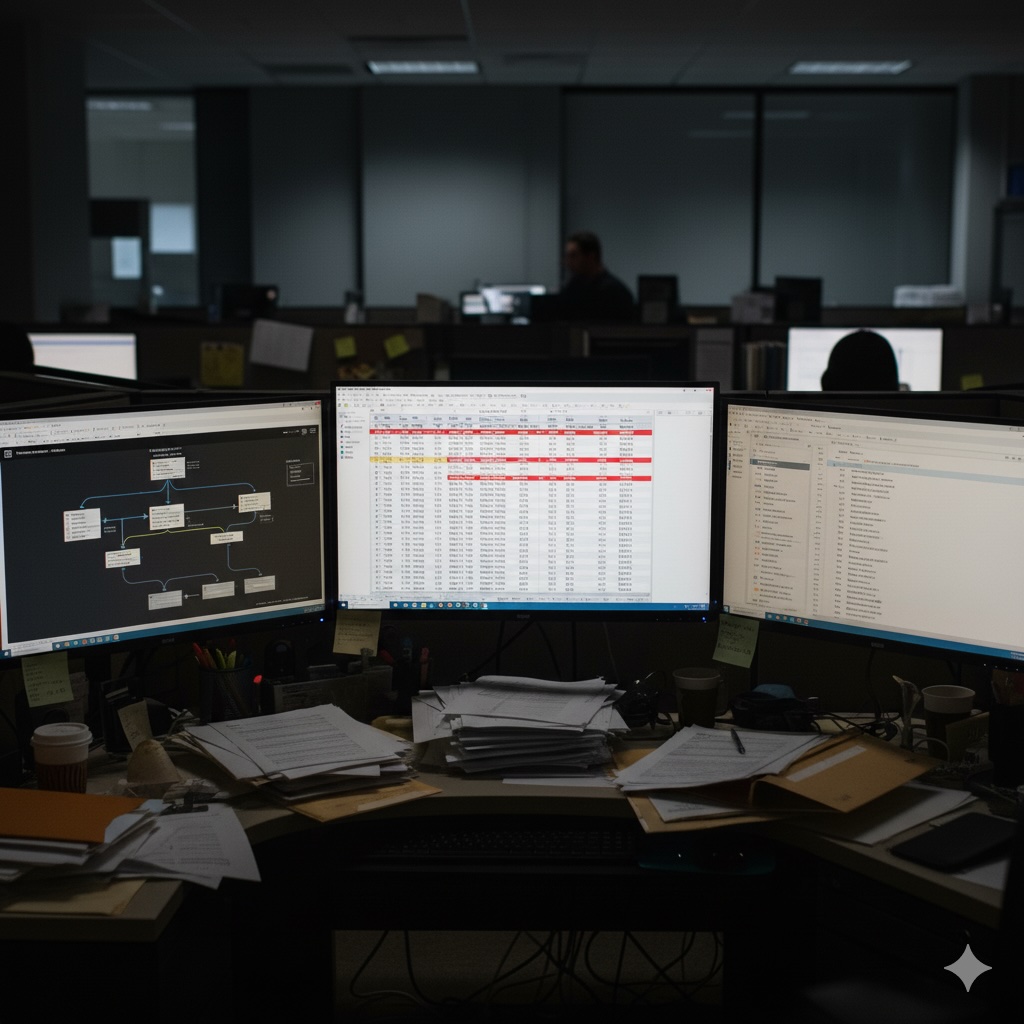
1. Reliance on Spreadsheets for EDI Monitoring and Exception Tracking
Far too many payers still track the status of inbound and outbound EDI files using spreadsheets. It may start simple, but as volumes scale and business complexity increases (think multiple groups, trading partners, file types, rejections, and splits), Excel monitoring quickly grows into a source of risk, inefficiency, and anxiety.
- Hidden Costs: Manual logs miss files that never arrive, can’t catch late transmissions in real-time, and can easily introduce human error that leads to delayed claims or eligibility.
- Fragmented Accountability: Multiple teams add their own columns and tabs, creating finger-pointing during issues and audits.
- Zero Scalability: As transaction volume grows, updating spreadsheets becomes unmanageable, and nobody wants to be on-call for late-night spot checks.
Eliminating spreadsheets is a critical first step to reliable EDI integration. What actually works?
- Centralized Real-Time Monitoring: Solutions like EDI Sumo bring all your file exchanges, across every format (EDI 834, CSV, XML, you name it), into a unified dashboard. No more hunting for yesterday’s files or racing to catch up with exceptions; it’s all tracked in real time for the entire team.
- Automated Alerts: If a file is late, missing, or failed, the system notifies the right people instantly.
- Role-Based Access and Audit Trails: End users, IT, EDI, compliance—all get the access they need, while a full history of data movement and user actions is captured for later review.
2. The Growing Cost of SLA Penalties
Service Level Agreements (SLAs) are unforgiving in the world of healthcare EDI. When claims or eligibility files are processed late or missed, it’s not just patient/member frustration you risk; it’s substantial financial penalties and damage to your contractual relationships.
- Why It’s So Easily Overlooked: With fragmented systems and a lack of real-time file monitoring, issues are detected after the fact, when penalties are already assessed by groups, TPAs, or employers.
- Growing Risk Profile: Health plans facing shrinking margins simply can’t afford the hit, especially when penalties are measured in six or even seven figures over the course of a year.
- Downstream Impact: Late claims lead not only to direct fees, but also delayed reimbursement, member confusion, escalated calls, and stress for Customer Service and IT teams alike.
What do high-performing payers do differently?
- Automated SLA Tracking: File exchanges and claim processing are monitored in real-time, so delays or failures are immediately caught and corrected, pre-empting most issues before penalties accrue.
- Performance Dashboards: Teams can see at a glance how their operations are trending against SLA targets, making it easy to spot and address chronic problem areas.
- Data Standardization: Ensuring every incoming and outgoing file matches the required standard makes compliance not an afterthought, but a baked-in part of the workflow. This keeps your plan in good standing, reduces remediation work, and protects revenue.
3. Manual EDI Exception Handling: The #1 Resource Drain for IT
Every payer IT team knows the drill. A mismatched record, a missing dependent, an out-of-spec segment, and suddenly you’re hand-editing files or manually contacting trading partners. Exception handling has become the biggest unsung resource drain in health insurance operations.
- Non-Stop Interruptions: Instead of improving systems, IT is stuck firefighting. This pulls technical staff away from innovation and piles on burnout.
- Slow Root-Cause Resolution: When every exception or file rejection gets handled ad hoc, patterns are missed. The same errors get fixed multiple times rather than being prevented.
- Increased Support Calls: Downstream impacts hit customer service and operations, as bad data creates more member questions, claims, and reprocessing needs.
The shift from reactive to proactive exception management is possible if you have the right process support:
- Automated Error Detection: Proactive solutions automatically identify any anomalies, outliers, or standard violations (WEDI/SNIP Levels 1-7) as soon as they’re received.
- Custom Validation Rules: Being able to set payer- or group-specific validation checks keeps files clean, personalized to the business lines you actually serve.
- Unified Dashboard for Exception Tracking: With all errors, exceptions, and resolutions tracked in a single place, teams can spot trends, improve processes, and cut out repetitive manual work.

4. Missed Files, Missed Revenue
It’s dangerous to assume no news is good news in EDI. Many health plans have discovered that files they thought were flowing never actually reached their destination. Or perhaps files aged in an exception queue for too long and created months’ worth of hidden compliance risk.
- Missed Enrollment and Claims Files = Missed Revenue: Without real-time visibility, enrollments don’t update, claims aren’t generated, and premiums or reimbursements slip through the cracks.
- Compliance Blowback: Regulations require transparent, auditable data exchange. Missed files often translate into findings, fines, or even lost business upon review.
- Support Burden: Members and brokers experience unexpected eligibility or denied claims due to data lag. Customer Service teams spend their days triaging problems that should never have occurred.
The solution: End-to-end visibility and proactive exception management. Here’s how modern payers are achieving this:
- Real-Time Monitoring and Alerts: Full oversight of all file movements. If something ages in the process (waiting on correction, in an exception state, or simply not received), teams are notified immediately.
- Automation of Aged File Management: Automatic escalation for files that age beyond defined thresholds, keeping an audit-ready trail of action and status.
- Member and Claim Lookup: Customer service and support teams have instant visibility into the current status of any member, claim, or dependent, empowering them to resolve questions in minutes, not days.
5. Data Format Mayhem
Healthcare payers (and their trading partners) aren’t purely EDI shops. On any given day, you’re likely to juggle:
- X12 EDI formats (834s, 837s, 277s, 999s, etc.)
- Excel and CSV files from brokers, smaller employers, or TPAs
- XML, APIs, and positional files
- Flat-file extracts from legacy systems
Trying to normalize and reconcile all these formats by hand is a herculean task. Small mapping mistakes can introduce huge downstream problems from eligibility breakdowns to claim denials.
- Why Standardization Matters: Clean, interoperable data is the foundation for fast, accurate claims and hassle-free compliance.
- The Real Challenge: Most point solutions can’t handle all these formats; custom scripting is error-prone and tough to scale as business grows.
What works for modern health plans:
- Multi-Format Ingestion Engines: You need a solution that takes all the raw data (EDI, CSV, XML, etc.), applies robust validations, and standardizes the output, automatically.
- Seamless Integrations: The resulting, clean data should flow instantly into core systems—eligibility, claims, customer service—without waiting on nightly batches or manual reconciliation. EDI Sumo, for example, was specifically designed for this challenge-see our integrations page for the real depth.
- Downstream Automation: Automated reporting, trading partner returns (eg. 999 or 277 files), and system updates keep the info fresh everywhere it’s needed.
6. Security and Compliance: Audit Pressure Never Sleeps
PHI (Protected Health Information) security is only getting more critical. Regulatory requirements like HIPAA (and increasingly, GDPR) demand:
- Strong data encryption in transit and at rest
- Complete audit trails showing who accessed or changed data, when, and why
- Granular access controls for different roles
- Real-time alerts for suspicious or unauthorized activity
The challenge is that legacy EDI setups often leave these requirements unmet, or require weeks of log research every time an auditor shows up. The best-performing payers embed these practices by design, such as:
- Robust Security Protocols: Adoption of asymmetric encryption, MFA, OAuth2, and mandatory secure transfer methods (like SFTP).
- Audit-Ready Architecture: All access and data changes are logged automatically, making it easy to demonstrate compliance instantly during reviews or investigations.
- Deployable On-Prem or Private Cloud: Some payers want complete control over data residency and security posture, which is why EDI Sumo can be installed on your own servers if needed. See our full Trust Center for more on this approach.
Building a Future-Proof EDI Integration Program
No two health plans are alike, but nearly all face variations of these pain points. As enrollment, claims, and reporting demands increase (and as more file formats and member groups come on board), the only way to scale is to standardize, automate, and give proper access to the people who need it.
- Dump the spreadsheets and manual file spot-checks
- End the cycle of SLA penalties and invisible EDI failures
- Give your Customer Service, Enrollment, and Claims teams actual visibility and control
- Automation = time back for IT, less confusion for your stakeholders, and a better audit/compliance posture for the business
Ready to Fix Your EDI Pain Points For Good?
At EDI Sumo, we’ve worked with the entire range of payers, from smaller providers to multi-million-member health plans. Our platform was built to address these real-world pain points directly because we’ve lived them, too.
Want to see how centralized monitoring, automated alerts, exception management, and end-to-end data standardization can transform your operations, without a massive IT project? Take a look at our full solution suite or schedule a personalized demo. You’ll discover how to move from reactive firefighting to proactive, stress-free EDI management, all while driving down costs, compliance anxiety, and risk.
Your teams, your trading partners, and your bottom line will thank you.


.png)






.png)

.png)


.png)
