Designing Eligibility Dashboards for Non-Technical Teams: What Payers Actually Use Daily

Eligibility dashboards have become the heartbeat of daily operations for healthcare insurance payers. But when we have non-technical teams—enrollment directors, claims specialists, IT liaisons, and customer service representatives—relying on data every hour, usability becomes just as important as data accuracy. Drawing from our direct experience working with payers in vision, dental, and medical insurance, let’s go deeper into what matters most when building eligibility dashboards that are genuinely used by non-technical staff, every single day.
Why Non-Technical Teams Rely on User-Friendly Eligibility Dashboards
There’s a common pain point we see across healthcare payers: eligibility data floods in constantly through all sorts of sources—EDI 834 files, Excel and CSV sheets, XML files, and even direct system APIs. When access to this core information is locked away behind IT support tickets or complex queries, it frustrates front-line staff and slows down everything from error resolution to customer response time.
- Real-Time Access: Customer service reps and enrollment managers need to view up-to-the-minute eligibility without delay. Real-time data means fewer errors and faster answers.
- Self-Service Data Lookup: Instead of relying on IT to pull or interpret files, non-technical users need direct access to eligibility details, status history, and documentation.
- Proactive Alerts: Teams benefit from instant visibility into discrepancies or data quality issues, empowering them to take corrective action swiftly.
- Compliance Confidence: Automated, documented reporting and audit trails are non-negotiable for HIPAA and regulatory requirements.
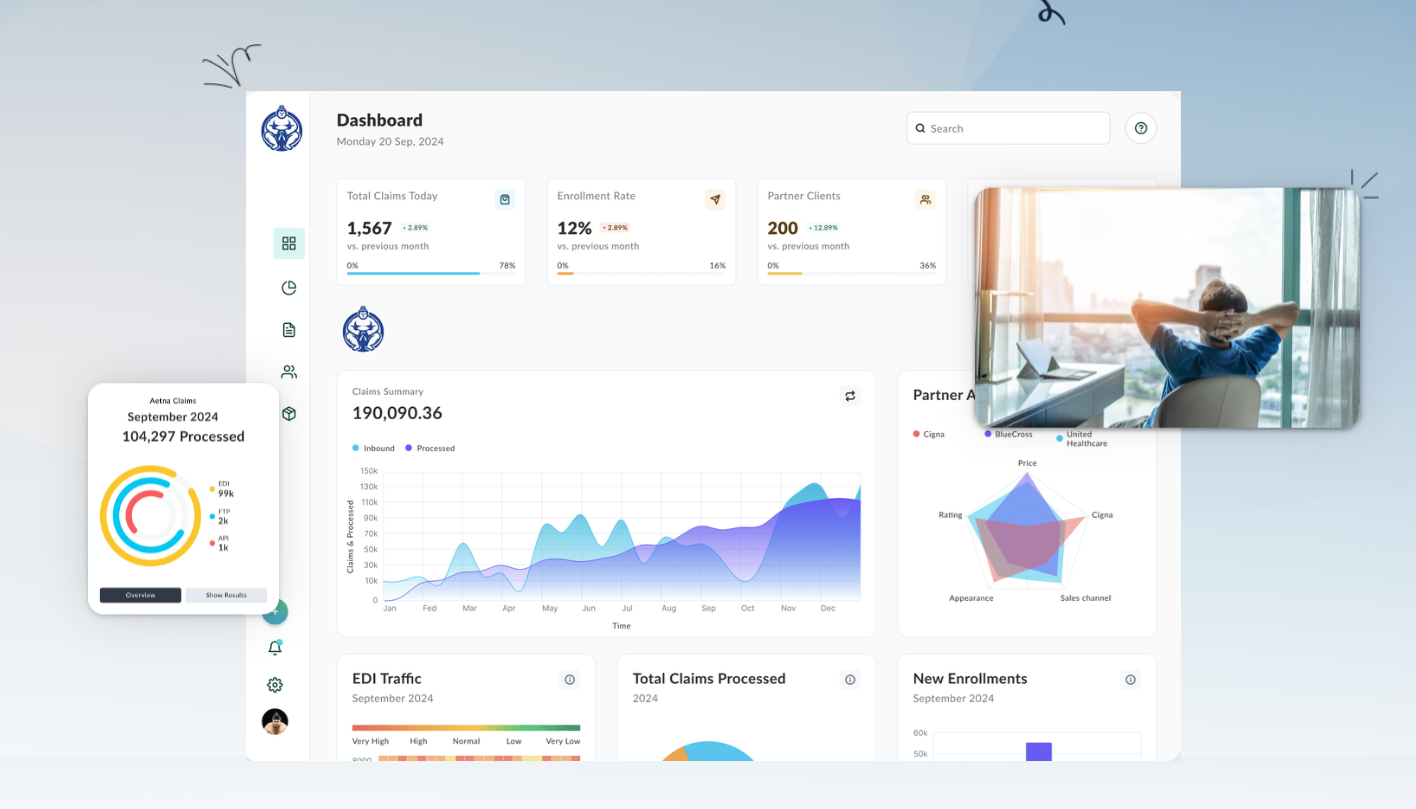
What Features Do Payers Use Daily?
From our conversations with enrollment and claims teams, here are the features that truly get used every day:
- Live Data Refresh: Non-technical staff need peace of mind they’re working with the latest data, eliminating confusion caused by outdated spreadsheets or static reports.
- Full Audit History: It’s critical to see who made what change, when, and why—especially when verifying eligibility retroactively or researching disputes. Audit trails support compliance and accountability.
- Error & Discrepancy Flags: The dashboard should highlight anomalies like missing fields, duplicated enrollments, or eligibility gaps, and notify the right person immediately.
- Clear Visual Indicators: Color-coded status (for example: green for active, red for terminated, yellow for pending/incomplete) makes it easy for users to grasp member status at a glance. Dashboards should prioritize filtering and sorting (group, region, date, etc.) so key metrics are never buried.
- Role-Based Views: Different teams need different dashboards. For instance, customer service focuses on fast lookups, claims on accurate submission histories, while directors require aggregate views for analytics and reporting.
- Multi-Format Data Standardization: The real world isn’t always EDI. Supporting uploads and standardization from various file types (EDI 834, CSV, XML, etc.) saves hours by removing the friction of file conversion.
- Compliance Dashboards: Automatic compliance checks and reporting make it straightforward to monitor HIPAA or state file requirements, reducing audit stress.
- Instant Exports & Reporting: With a click, staff should be able to generate Excel, PDF, or direct system integration reports for performance monitoring and regulatory response.
Designing Dashboards: Our Practical Approach
Building dashboards that become the go-to daily tool for non-technical teams involves blending empathy, workflow knowledge, and technical best practices. Here’s our blueprint:
- User Research: Speak to your claims coordinators and enrollment specialists first. Discover which data elements and workflows they touch most and where bottlenecks occur. Without this, any dashboard risks focusing on irrelevant metrics.
- Define & Build Role-Specific Views: Start with templates for each department, including customer service, enrollment, claims, and directors. Each view should prioritize what’s mission-critical for that role while hiding unnecessary complexity.
- Automate Data Ingestion: Connect all your source systems (EDI inflows, spreadsheets, SFTP, APIs) so users aren’t left wrangling files. Data validation and standardization should be automatic, with real-time updates whenever possible.
- Accessibility First: High-contrast palettes, multiple status indicators beyond just red/green, and compliance with ADA standards are musts for real-world teams. A dashboard isn’t truly user-friendly if not everyone can use it.
- Pre-set Templates & Defaults: Non-technical users shouldn’t be greeted with blank screens. Instead, offer templates (for example, “Active Members in My Group,” “Recent Error Flags,” etc.) that can later be customized.
- Pilot & Train: Early involvement of end users prevents costly re-do’s later. Keep training short and focused (20–30 minutes per role). Gather initial feedback, observe real-world use, and adjust the UI accordingly.
- Continuous Feedback Loop: Encourage teams to report confusing sections or suggest improvements right in the dashboard. Product owners should meet monthly to act on this input for continual evolution.

Design Details: Clarity, Simplicity, and Reliability
When we roll out new dashboards to clients, the feedback we get most often concerns clarity of layout, context for every data point, and reduction of clutter. Here are a few details we’ve learned are essential:
- Information Hierarchy: Lead with the most critical data (total active members, new enrollments, flagged issues). Less-used metrics can be placed in collapsible sections or advanced tabs.
- Quick Filters: Simple, large filters and search bars enable users to focus on their region, group, or coverage type with zero hassle.
- Contextual Tooltips & Help Prompts: Embedded explanations reduce support requests and boost user confidence.
- Mobile Compatibility: When remote or hybrid work is involved, dashboards should render cleanly on tablets and smartphones, not just desktop screens.
- One-Click Export: Exporting filtered results for regulatory, management, or audit use is a daily ask. Make it truly one click.
Security and Compliance: Non-Negotiables
Eligibility data is some of the most sensitive information handled inside a payer organization. We only expose it through dashboards that ensure:
- Full data encryption both in transit and at rest.
- Role-based and granular access controls, with support for authentication standards like OAuth2 and multi-factor authentication (MFA).
- Complete audit trails that log user actions for HIPAA compliance and easy retrieval during audits.
- Data standardization across all supported formats (EDI 834, XML, CSV) so front-line teams work from a single source of clean, harmonized data.
Lessons Learned from Real Teams
Our discussions with health insurance payers have made it clear: dashboards become business-critical tools only when built cooperatively with the people who will use them day after day. If you want high adoption rates and fewer support tickets, never overlook:
- Iterative Prototyping: Don’t launch and leave; continue to involve users post-launch for enhancements.
- Training Champions: Identify dashboard super-users in each department who can train others and provide grassroots feedback.
- Meaningful Metrics: Avoid flooding dashboards with vanity KPIs. Stick to actionable insights that help teams make better decisions faster.
This approach helped our partners move from IT bottlenecks and manual interventions to streamlined, proactive eligibility management.
Evaluating Tools for Non-Technical Use
When choosing tools for eligibility dashboards, always test with actual non-technical users. Prioritize solutions that offer:
- Pre-built templates specifically for insurance use cases
- Drag-and-drop dashboard and report building
- Real-time audit trails, alerts, and compliance monitoring
- Straightforward integrations with your existing eligibility, claims, and group administration systems
- Full encryption and role-based security controls
Solutions like EDI Sumo are purpose-built for payers, supporting multi-format EDI, robust reporting, and real-time compliance monitoring. These attributes provide a true advantage when non-technical teams are required to manage eligibility day-to-day.
Connect the Dots: Automation Breeds Accuracy
Automating data validation, standardization, and proactive alerting is the key to error reduction. Removing manual touchpoints—uploading files, searching for errors, reporting statuses—frees up time and ensures data quality.
Bottom Line: Empower, Don’t Complicate
If it’s time for your organization to finally take eligibility (and the teams that rely on it) from chaos to clarity, you can always reach our experts for advice or a tailored demo.
Want to see eligibility dashboards in action for non-technical teams? Schedule a demo with EDI Sumo. We’d love to share what we’ve learned and help you achieve operational clarity.


.png)






.png)

.png)


.png)
