The Eligibility Playbook for January Surges: How Payers Keep 270/271 Stable Under Peak Load


Every January, as open enrollment deadlines approach and the calendar turns, healthcare payers brace for one of the most demanding periods of the year: the eligibility verification surge. The spike in EDI 270/271 transaction volumes can double or even triple overnight, pushing existing systems and teams to their absolute limits. At EDI Sumo, we have seen up close how savvy organizations prepare for this seasonal crush, keep eligibility pipelines stable, and mitigate downstream disruptions to claims, enrollments, and customer support.
Here’s the definitive playbook to ensure you keep operations smooth, compliant, and customer-centric during this high-stakes period.

Why January Surges Challenge the 270/271 Eligibility Ecosystem
Every payer (whether vision, dental, or medical) feels the pressure as member inquiries explode in January. High volumes are driven by new ACA plan selections, employer rollouts, and shifting Medicaid/CHIP eligibility policies. The sheer load exposes brittle systems and process gaps:
- Transaction spikes: Daily 270/271 volumes can rise 300%, sometimes overwhelming even well-staffed IT teams.
- Format fragmentation: Requests arrive in EDI, XML, CSV, and via APIs. The need for immediate 271 responses to confirm member status is overarching.
- SLA and compliance risk: Delays in processing can breach 24-hour SLAs and raise the risk of HIPAA non-compliance.
- Customer service strain: When real-time eligibility checks lag, call center volume balloons and claim denials soar.
It’s not just about technology but about systems thinking. When enrollment data is fragmented and manual workarounds become the norm, small errors ripple into larger financial and operational headaches downstream.
Anatomy of the 270/271 Workflow Under Pressure
The eligibility workflow in peak periods consists of several stages where bottlenecks can emerge:
- Ingestion: Receiving member eligibility requests from employers, providers, exchanges, and partners in multiple formats.
- Translation and validation: Converting files to a unified structure, applying custom business validations, and reconciling against internal systems.
- Response generation: Assembling accurate 271 responses and delivering back (often in real time).
- Exception handling: Flagging, routing, and resolving discrepancies, errors, or incomplete records before they affect downstream systems.
- Reporting and compliance: Maintaining real-time audit trails, dashboards, and alerts to track performance and adherence to HIPAA and organizational SLA requirements.
Gaps at any stage, from ingestion to compliance, can quickly result in eligibility uncertainty, claim denials, and regulatory headaches. The stakes are high because these workflows touch everything, from claims processing to member satisfaction and compliance exposure.
Playbook for Stability: 5 Steps to Bulletproof 270/271 in January
At EDI Sumo, our approach is both hands-on and holistic. Here are the steps we've seen work, drawn from software, process, and integration best practices gleaned from real payer environments.
Step 1: Multi-Format Ingestion and Automated Translation
No matter what format your eligibility inquiries arrive in (EDI, Excel, CSV, XML, or positional text), you must have automated translators to harmonize and standardize inputs immediately. This avoids downstream errors and ensures accurate, rapid response. We set up SFTP auto-pulls and API endpoints for trading partners, dramatically reducing manual uploads and human error. The goal isn’t just ingestion, but seamless conversion to a single internal standard.
Step 2: Real-Time Monitoring and Proactive Alerts
Real-time dashboards are indispensable. Aggregate live performance metrics: transaction volume, average response times, error rates, and SLA compliance. Embedded, automated alerts should flag anomalies—such as repeated transaction failures, abnormal traffic spikes, or recurring subscriber ID errors—before they escalate. At EDI Sumo, we alert teams via email and SMS right away when a data anomaly is detected, empowering IT and operational staff to resolve issues minutes instead of hours (or days!).

Step 3: Empower Role-Based Views From Enterprise to Agent
Eligibility processing touches multiple roles across payer organizations, from CIOs to Enrollment Directors to front-line Customer Service reps. We build role-based dashboards so the right people see the right data: enterprise-wide summaries for leadership, instant lookup and audit research tools for member services and IT, and granular error logs for technical staff. Instant, accurate eligibility data at every level supports a faster call resolution and gets members the answers they need on the first contact.
Step 4: Seamless Integration and Robust Validation
Breaks in eligibility workflow often happen when data flows between silos like eligibility, claims, and enrollment systems. We prioritize strong, standards-based integration to major platforms (including Guidewire, Aetna, Cigna, UnitedHealthcare, IBM Sterling B2Bi, and others cited in our work) and enforce custom SNIP-level validation so only clean, accurate data moves forward. This closes the loop and eliminates silent errors that might cause costly claim rework.
Our own eligibility solution supports SNIP Levels 1-7 for both compliance and business assurance, a topic we explore further in our guide to SNIP Level validation.
Step 5: Continuous Audit, Automated Reporting, and Compliance Scaling
No eligibility operation is complete without robust audit trails and automatic compliance reporting. All EDI 270/271 transactions are logged, tracked, and available for real-time reporting. Automated performance summaries, trading partner acknowledgments, and compliance dashboards should be designed to satisfy HIPAA and GDPR mandates. EDI Sumo’s architecture enables modular growth: start with eligibility, expand to claims and customer service insights, and stress-test regularly to ensure the stack can absorb 10x load increases.
Security is non-negotiable, especially with sensitive personally identifiable information. Advanced encryption (at rest and in transit), multi-factor authentication, and on-premises or cloud flexibility ensure your eligibility pipelines are not just fast, but safe.
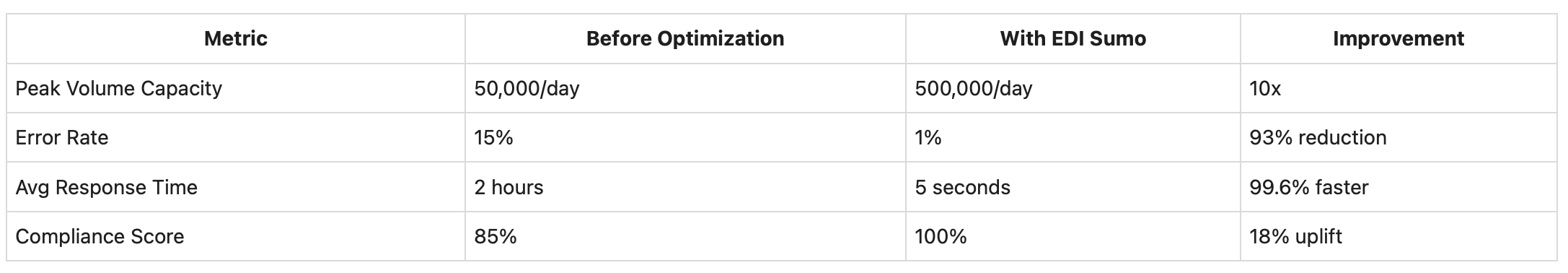
Metrics That Matter: Measuring Post-Peak Improvements
It’s not enough to just weather the January wave; you need to quantify you’re truly improving. Based on direct experience, here are the top metrics to benchmark:
- Peak daily volume supported (before/after): How many 270/271 files can you process in a single day without delay?
- Error/exception rate: What percentage of transactions require manual follow-up or cause downstream disruption?
- Average response time: How quickly are 271 responses returned, especially during surge?
- SLA and compliance adherence: Are you consistently within contractual and regulatory requirements?
Preparing for January: What Strategic IT Leaders Must Do Next
We find that CIOs and Enrollment Managers who work proactively save massive amounts of time and money come January. Here’s how:
- Run stress tests in Q4: Simulate 10x peak volume to find weaknesses before they hit production.
- Automate routine discrepancies: Set up logic to auto-resolve the most common eligibility errors based on historical data.
- Invest in training: Equip member services and IT teams with dashboards and audit tools before open enrollment hits.
- Keep clear escalation channels: With instant alerts and audit trails, incidents are routed to the right experts without delays.
This level of preparation means you’re not just surviving surge, but building trust with both members and trading partners who expect consistent, accurate eligibility answers.
January Eligibility Success Is Built Now
Peak load management for 270/271 isn’t just a January concern; it’s a litmus test for the strength of your eligibility, claims, and enrollment operations year-round. When you standardize formats, automate validations, enable enterprise visibility, and maintain proactive compliance, you create a foundation that can weather any surge and keep your organization ready for both current and future regulatory demand.
To explore how you can stabilize and modernize your eligibility processing, including real-time monitoring and multi-format support, visit EDI Sumo eligibility solutions. Get in touch with our team to discuss your specific goals and scheduling a tailored demo.


.png)






.png)

.png)


.png)
