The CIO’s Guide to Future-Proofing Healthcare EDI for Evolving Compliance and Interoperability Needs

Staying ahead of the curve in healthcare EDI (Electronic Data Interchange) isn't simply about compliance—it's about protecting your organization's operational agility for years to come. The rapid evolution of healthcare data regulations, growing needs for true interoperability, and the ever-present threat of security breaches mean CIOs and IT leaders must lay foundations today for the data demands of tomorrow.
At EDI Sumo, we've worked hands-on with payers of all sizes to standardize, secure, and make EDI and enrollment data both accessible and actionable, and we're sharing what we've learned about future-proofing your EDI strategy.

Why Future-Proofing EDI Matters Now More Than Ever
Healthcare IT and EDI environments are changing faster than at any time in the past two decades. CIOs are being squeezed by:
- Constantly evolving HIPAA and other compliance requirements—A routine audit can reveal gaps overnight.
- More connections, more formats—Plan sponsors, partners, employers, exchanges, and regulators each demand different file types and communication protocols.
- Exponential data growth—Payers process millions of records; manual mapping, validation, or error correction simply doesn’t scale any longer.
- Demands for transparency—Business leaders want claims, eligibility, and enrollment data visible on-demand, not hidden behind technical silos.
Without a strategy built for continuous change, EDI investments risk becoming brittle, opaque, and a drag on core payer operations.
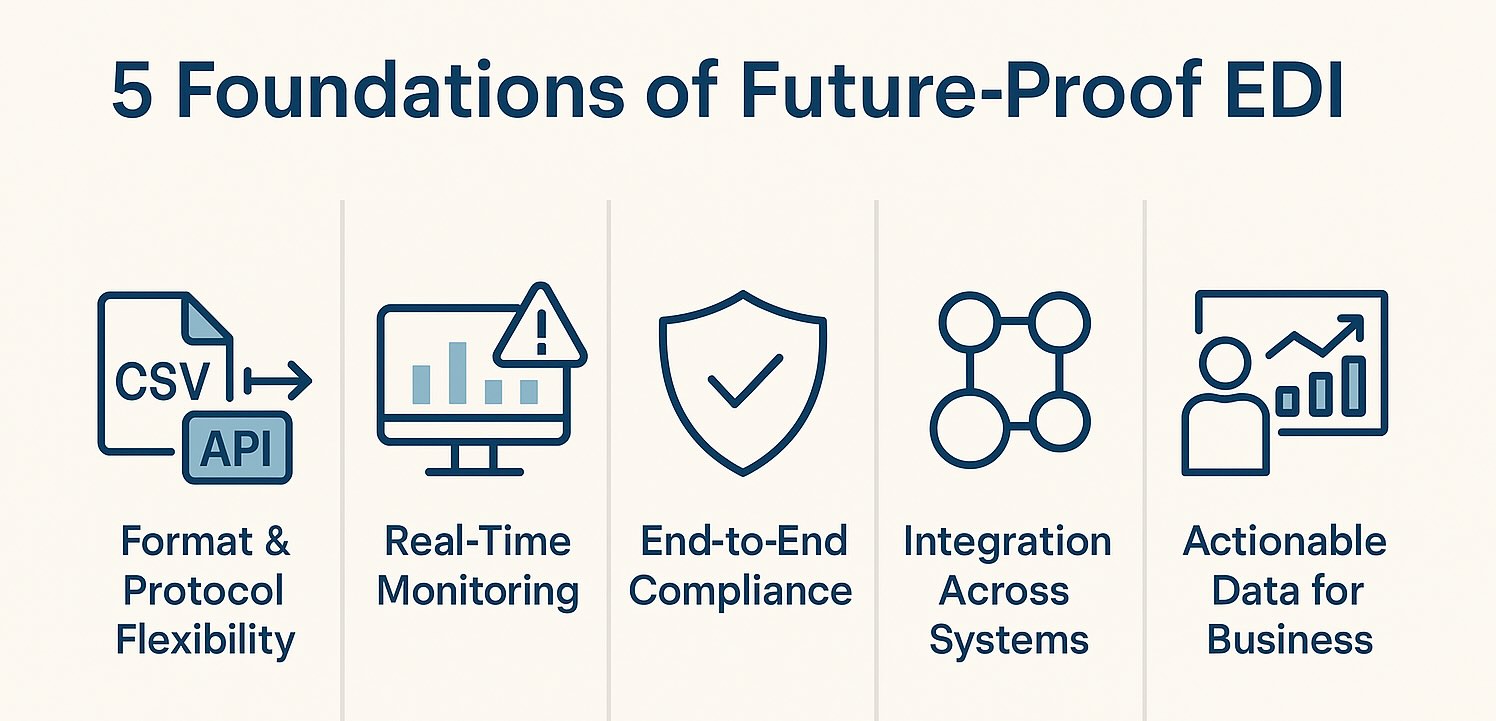
Critical Foundations for CIOs: How to Future-Proof Healthcare EDI
1. Embrace Format & Protocol Flexibility
The reality for payers is that you’ll face every data input under the sun—from legacy EDI (like 834 and 837), XML, CSV/Excel, positional flat files, to new APIs. Your EDI platform must:
- Support multi-format and omnichannel ingestion without manual mapping for each new trading partner.
- Enable one-click standardization and validation for any format—regardless of source or downstream destination.
- Provide configurable rules to easily onboard new clients, employer groups, or lines of business, avoiding expensive custom code or brittle scripts.
At EDI Sumo, we help payers eliminate the endless mapping treadmill with tools for format-agnostic data processing. The result: IT teams reclaim countless hours, and business teams get the data they need faster.
2. Prioritize Real-Time Monitoring & Accessibility
Historically, EDI systems were black boxes. Today, IT and business teams cannot wait days for error reports, especially when lives or claims dollars are at stake.
- Real-time dashboards should surface current eligibility, claims, and transaction status.
- Automated alerts and notifications empower teams to address discrepancies instantly—slashing turnarounds and avoiding costly penalty fees.
- Empower your support teams, not just your back-end specialists: customer service solutions let staff access member and claim information in-the-moment, accelerating resolutions.
3. Strengthen End-to-End Compliance & Audit Readiness
Regulatory change is a guarantee—from updated 5010 standards, to enhanced privacy controls in HIPAA, to local regulations like GDPR for global payers. Future-proofed EDI means:
- Real-time audit trail generation, with traceable logs for every data change, view, and transfer.
- Configurable validation layers for WEDI/SNIP levels, custom client rules, and new payer requirements—without repeated system changes.
- Automated compliance reporting that can be delivered to regulators or plan sponsors in minutes, not weeks.
At EDI Sumo, our Trust Center details how we help clients stay HIPAA compliant and audit-ready around the clock.
4. Architect for Integration Instead of Isolation
Payer organizations rely on a tech ecosystem: claims management systems, CRM platforms, payment systems, and more. EDI data should flow seamlessly between these, not live in silos managed by tired IT teams.
- Support out-of-the-box and custom integrations with systems like Guidewire, Aetna, Blue Cross Blue Shield, and others (see our full integration catalog here).
- Enable secure, standardized APIs or SFTP transfers to keep downstream processes moving in real time.
- Leverage role-based access to ensure security as teams from different departments tap into EDI data.
5. Make Data Actionable for the Business—Not Just IT
The ultimate power of EDI isn’t in the format or the technology—it’s the business outcomes it enables. Payers who win in the future will:
- Put standardized, validated EDI data at the fingertips of operations, support, finance, and compliance—not just developers.
- Empower customer support to resolve eligibility or claims questions with instant lookups and discrepancy alerts.
- Use enhanced audit trails and reporting to defend against audits, reduce fraud, and improve member satisfaction.
- Shrink the load on IT teams, freeing them for innovation rather than reactive issue-fighting.
Building on Modern Security and Privacy Practices
All future-proofing plans hinge on protecting member data. Today's—and tomorrow’s—threat landscape demands:
- Asymmetric encryption for data in transit and at rest—keeping all claims and eligibility records tightly secured.
- Compliance with the latest standards, including HIPAA, GDPR, and state-specific regulations.
- Complete auditability and role-based permissions, with support for OAuth2 and MFA for system access.
As threats evolve, these capabilities are baseline, not advanced. EDI Sumo's security framework is designed from the ground up for healthcare payers and sensitivity of EDI data flows.
Proactive Monitoring: The EDI Advantage No CIO Should Ignore
Lapses in eligibility processing or claims errors can lead directly to blown SLAs and compliance fines. With real-time monitoring, our clients have reported:
- Consistently meeting and exceeding service level agreements
- Up to 45% acceleration in claims processing cycles
- Near elimination of data lag—moving from batch processing to near real-time visibility
Whether you're a CIO, EDI coordinator, or enrollment and claims leader, imagine what your team could do with proactive, actionable EDI monitoring, automated alerts, and intuitive dashboards—without ripping and replacing your core systems.
Preparing for the Next Wave of Interoperability
As federal and industry moves push for greater interoperability—think of CMS’s rules around patient access APIs and payer-to-payer data exchange—the bar for agility will only rise. Your EDI solutions should:
- Handle new API-driven exchange protocols with the same confidence as legacy transactions
- Allow flexible addition of new data trading partners without new buildouts
- Surface and standardize data for use across every business unit in your organization
With true integration and interoperability, you’re not just compliant: you’re more competitive and responsive to every stakeholder.

Key Questions CIOs Should Ask to Future-Proof EDI
- Can my platform natively support all required data formats and rapidly onboard new partners—without custom code each time?
- Will my business users get real-time file, claim, and eligibility visibility and incident notifications—not just siloed batch reports?
- Are my compliance, audit, and security logs generated and exportable in real time, across every EDI interaction?
- Do my systems integrate with existing and future claims/enrollment platforms, enabling seamless data flows—regardless of underlying tech?
- Does every stakeholder—from support to compliance—have access to the data they need to perform at their best?
Why Start the Conversation Now?
Healthcare EDI isn’t standing still—and neither can your strategy. Whether you’re confronting a migration from a legacy platform, needing to ensure HIPAA compliance ahead of a looming audit, or looking to empower your teams with better, faster, more actionable EDI data, now is the time to assess your approach.
With EDI Sumo as your partner, we streamline and automate multi-format enrollment, claims, and eligibility processes, integrate data enterprise-wide, and ensure you meet compliance and SLA targets with confidence. And crucially, we put actionable data and tools in the hands of the end users who drive real outcomes.
Ready to future-proof your EDI environment, bring agility back to your IT teams, and turn compliance into a competitive advantage? Let’s talk about your needs and schedule a demo. Your organization’s next decade of EDI innovation starts with the choices you make today.


.png)




.png)

.png)


.png)
