Modernizing Healthcare Payer Systems: Using AI and Machine Learning to Improve EDI Data Quality

Healthcare payers are at a critical crossroads. The explosive growth of electronic data interchange (EDI) in the insurance sector has improved the transmission of eligibility, claims, and enrollment information. However, supporting complex EDI standards (like 834, 837, 277, and 990) and a variety of file formats (Excel, CSV, XML, and more) continues to strain IT resources. In an industry juggling razor-thin margins, regulatory scrutiny, and expectations for near-real-time data, even minor errors can snowball into compliance breaches, SLA penalties, or delayed patient care. This is where the strategic integration of AI and machine learning fundamentally reshapes the game.
Why EDI Data Quality Is So Hard, And So Critical
Legacy payer systems were designed in an era where overnight batch processing and rigid file standards sufficed. As payers grew via mergers, new business segments, and partnerships, their data landscapes became exponentially more complex. Today, most organizations ingest and exchange member and claims data from a dizzying array of file types, often with incomplete or ill-formatted information that threatens data integrity. Poor quality in EDI data can result in:
- Delayed claims payments, member onboarding, or eligibility activation
- Manual rework that drains IT and support teams
- Inaccurate reporting, risking compliance with HIPAA and other mandates
- Frustrated customers and providers unable to access real-time information
Traditional rules-based EDI engines are brittle and resource-intensive—any deviation, whether a stray format or a population-specific data quirk, can bring processing to a halt. If the future of payer operations is data-driven and automated, a more adaptive, intelligent approach to data quality is non-negotiable.
The AI and Machine Learning Difference
Let’s get practical: AI and machine learning allow us to move beyond thousands of static data validation rules toward models that recognize, learn, and adapt to new data patterns, even as trading partners, regulatory rules, and member expectations change. Here’s how these technologies are redefining EDI data quality for healthcare payers:
1. Format and Schema Intelligence
AI-driven systems can ingest data from any source—834s, 837s, CSVs, XML, or positional files—and automatically detect structure, normalize naming conventions, and even correct common formatting issues on the fly. This flexibility is essential when onboarding new groups or partners, or dealing with decades of legacy process variation.
2. Anomaly Detection in Real Time
Machine learning algorithms can flag records that deviate from baseline patterns—not just for missing fields, but for complex, context-dependent errors. For example, if a member is flagged as eligible with one effective date sequence in one feed but contradicted in another, or if claim lines show unexplained outliers, the AI surfaces these issues instantly rather than after costly downstream impact.
3. Automated Root Cause Analysis
Instead of simply flagging errors, modern solutions leverage AI to trace issues back to their origins. Was the issue in the incoming file, a mapping/transformation error, or a systemic problem with a particular trading partner? With these insights, payer IT and business teams can proactively correct sources of error before a backlog builds up.
Real-World Benefits: Efficiency, Compliance, and Member Experience
- End-to-End Automation: AI-powered data checks run as files arrive, catching errors before they reach claims or member systems. This drastically reduces manual intervention and expedites onboarding, eligibility checks, and claims cycles.
- Continuous Learning: As more data flows through the pipe, machine learning models sharpen their ability to differentiate between acceptable variances and real errors—reducing false positives that can bog down support teams.
- Audit-Ready Compliance: Advanced systems like EDI Sumo generate real-time audit trails, supporting HIPAA and GDPR requirements without painstaking data extractions or after-the-fact forensic reviews.
- Proactive SLA Management: Automated alerts and performance dashboards enable payers to stay ahead of SLA risks, preventing penalties and enhancing relationships with employer groups and trading partners.
What Makes Modernizing Payer EDI Unique at EDI Sumo?
At EDI Sumo, we’ve built our solutions with exactly these pain points and innovations in mind—this isn’t academic AI, but battle-tested automation that makes a tangible impact for healthcare payers
- Multi-Format Support: We process EDI 834, 837, CSV, XML, and more—removing guesswork and minimizing manual mapping when onboarding new groups. Eligibility Processing is vastly streamlined as a result.
- Real-Time Monitoring and Error Detection: Our modular architecture can track each transaction, detect anomalies instantly, and issue actionable alerts. This is crucial for meeting and exceeding SLAs.
- Compliance by Design: With built-in, real-time audit trail generation and robust reporting modules, we make it easier to stay HIPAA-compliant and audit-ready—always.
- Seamless Integration: EDI Sumo connects with existing payer systems—from claims management to modern EDI translators—maximizing investments in legacy infrastructure while ushering in AI-enabled modernization.
Step by Step: How AI Improves the Workflow
- File Ingestion: Support for virtually any file type/format, with automatic detection and pre-mapping
- Schema Validation: AI ensures that all critical fields meet payer-specific and industry-standard rules, adapting as new variations emerge
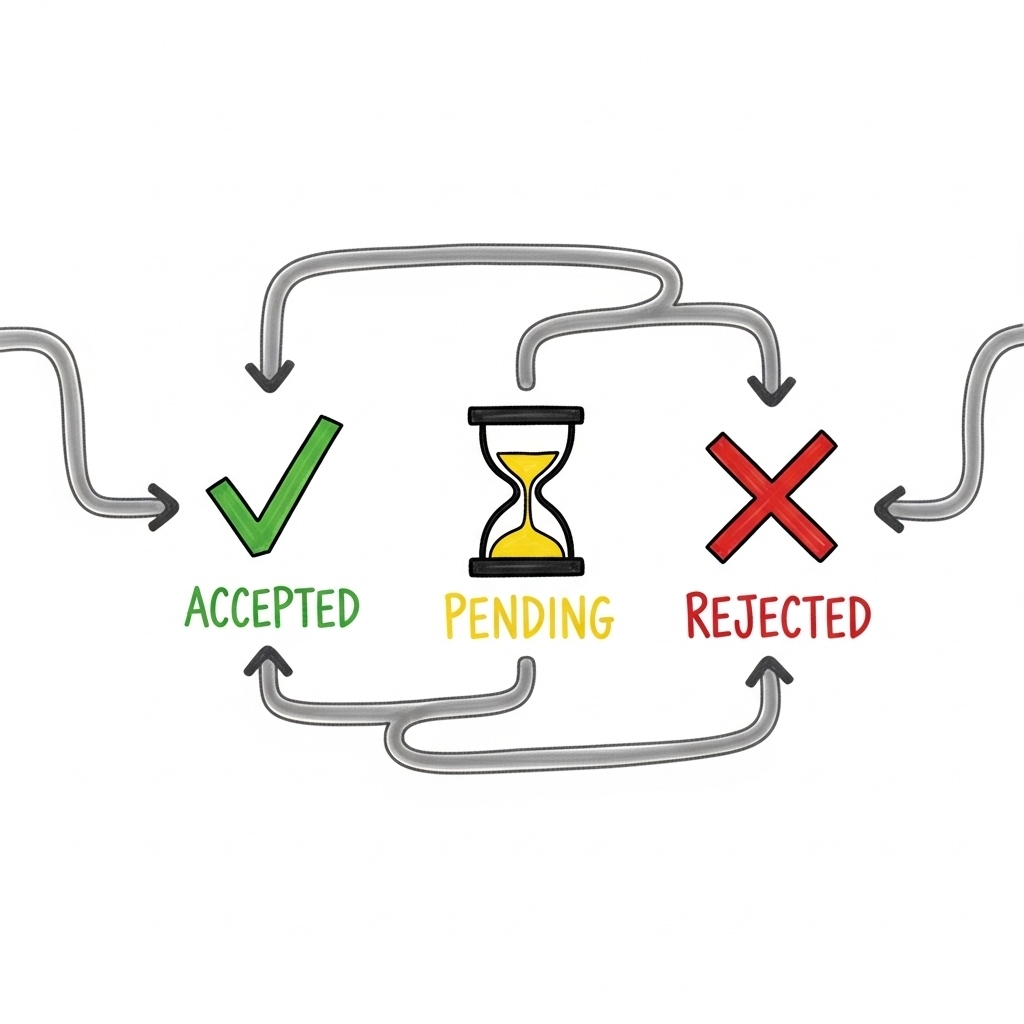
- Anomaly Identification: Issues ranging from missing effective dates to unrecognized group codes are surfaced immediately, helping teams react before files hit core claims or enrollment systems
- Resolution Guidance: Root cause and suggested next steps are provided, closing the loop between IT, support, and business teams
- Continuous Feedback Loop: The platform learns from resolved issues, getting sharper at identifying and auto-correcting repeat problems
Human in the Loop: Empowering IT and Support Teams
Importantly, AI and machine learning are not about removing the human element from payer operations. Instead, they are force multipliers—empowering IT and support staff to focus on high-value work by minimizing time spent hunting for data errors or fixing preventable problems. Real-time dashboards and self-service data access put actionable information back in the hands of business users, instead of locking it behind IT tickets and batch job queues.
Security and Trust: Key Pillars for Modern EDI Modernization
Security cannot be an afterthought, especially as payers centralize sensitive EDI data. EDI Sumo employs advanced asymmetric encryption, strict role-based access, and complete audit logging to give customers peace of mind. Whether data privacy regulations tighten or new audit frameworks emerge, you’ll be ready.
Getting Started: What Does AI-Enabled EDI Modernization Deliver?
- Cleaner, more trustworthy enrollment and claim data from day one
- Reduced manual intervention and faster onboarding for new partners/trading groups
- Fewer SLA penalties, denied claims, and rejected eligibility records
- Confidence to pass audits and report accurately without late nights or fire drills
- Support teams who can answer member questions rapidly, based on reliable, real-time data
The true power of AI and ML in healthcare payer EDI isn’t theoretical—it’s practical, immediate, and begins to pay off as soon as you move beyond manual QC and static rules engines. Our approach at EDI Sumo is about meeting you where you are, integrating with your current stack, and giving you confidence that every byte, from eligibility to claims, will be accurate, compliant, and ready when you need it
If you want to see how intelligent automation and EDI modernization can transform your claims, enrollment, and support processes, explore our solutions or schedule a demo. Let’s put data back in your hands and unlock the next era for your healthcare payer organization.


.png)




.png)

.png)


.png)
