KPIs That Matter for Electronic Payments: From Days-to-Pay to Touchless Rates


For healthcare payers, IT directors, and enrollment leaders, electronic payment processing is the engine of cash flow and member satisfaction. It promises to eliminate costly bottlenecks and reduce manual labor, but how do you know if your system is actually delivering on that promise? Simply tracking the volume of claims paid isn't enough. We're breaking down the critical Key Performance Indicators (KPIs) that truly measure the health, efficiency, and compliance of your electronic payment workflows. Stop focusing on vanity metrics and start tracking the numbers that directly impact your bottom line and operational resilience.

Why Payment KPIs Matter in Healthcare Payer Operations
In healthcare, electronic payments are the bridge between data quality, operational efficiency, and compliance. Every claim, enrollment, or status update—whether delivered via an EDI 834, 837, 277, or 999 file—represents complex data that must be standardized, validated, tracked, and ultimately paid. Getting KPIs right is not a theoretical exercise. It’s about:
- Ensuring accurate, compliant, and timely payments to providers and members
- Minimizing manual interventions that slow processing and increase costs
- Maintaining real-time visibility into cash flow and bottlenecks
- Protecting your organization from penalties due to non-compliance
Our experience tells us that when metrics are clearly defined and measured, payer teams can confidently move from putting out fires to proactively improving both member and provider experiences.
1. Days-to-Pay: The True Test of Efficiency
Days-to-pay is one of the most telling indicators for any electronic payment process. It measures the elapsed time from when a payment is initiated (such as an EDI 837 claim) to when funds are settled or made available to the recipient.
- Industry Context: Manual workflows often result in days-to-pay stretching to 7-10 days. Streamlined electronic processes typically bring this down to 2-4 days for most claims and enrollments.
- Why it Matters: Shorter days-to-pay means faster provider reimbursement, fewer provider calls, and improved satisfaction. Plus, it frees up working capital for your plan.
- Best Practice: Use automation and standardization across all data formats to drive days-to-pay lower, and maintain audit trails for every transaction step.
You can learn more on why speed matters in claims by exploring The Impact of Real-Time Eligibility Verification on Claims Processing Speed.
2. Touchless Rate: How Much Is Truly Automated?
Touchless processing rate defines the percent of transactions that move from intake to completion with zero manual intervention. In high-performing payer operations, this is the hallmark of process maturity.
- Our perspective: In complex payer settings with varied file formats (EDI, CSV, Excel, XML), true touchless automation requires robust validation and flexible integration. Solutions like EDI Sumo enable organizations to consistently achieve high touchless rates, especially for transactions that are clean or match against purchase orders or master provider data.
- Why it Matters: Every transaction that doesn’t require a human touch reduces error risk, operational overhead, and processing time.
We encourage tracking touchless rates both holistically and by transaction type. For example, high rates on EDI 834 or EDI 837 files can indicate that your standardization and validation workflows are mature.
3. Error and Exception Rates: Spotting Friction Early
Exception rate and error rate are not just technical metrics. They are leading indicators of process health.
- Exception Rate: Percent of transactions that cannot be processed automatically and require manual intervention (often due to data mismatches, formatting, or missing information).
- Error Rate: Percent of transactions that fail validation or are outright rejected, often triggering a need to send a 999 or 277 response in the EDI ecosystem.
Best-in-class payer organizations drive exception rates below 2%. This requires not only strong validation, but also the ability to view error patterns by trading partner, format, or internal workflow.
4. Authorization and Acceptance Rates: Getting Approvals the First Time
Authorization rate is the percent of payment or enrollment transactions that are approved on first pass. Acceptance rate widens the lens to include transactions that initially failed but were successfully resolved on retry.
- For health insurance: High authorization rates on EDI 834 enrollments or EDI 837 claims tell us that most records conform to required standards (WEDI/SNIP, payer rules).
- Aim for: 90% or higher on both metrics. If you’re consistently lower, it’s a signal to review and strengthen your validation, member data quality, or trading partner onboarding.
Our platform’s cross-format validation and real-time alerts are designed to help payer IT and operations teams achieve the highest possible rates, minimizing downstream corrections.
5. Compliance and Audit Metrics: What Regulators Will Ask
KPIs like audit trail completeness, SNIP level adherence, and HIPAA compliance are not just for peace of mind. They’re critical to passing audits and avoiding penalties.
- Audit Trail Completeness: Track the percent of transactions with a full record of every system and user action. This is essential for compliance, dispute resolution, and operational learning.
- SNIP Level Compliance: Monitor percent of claims or enrollments passing each required SNIP validation. In practice, this protects you from downstream issues and strengthens your trading partner relationships.
- HIPAA Compliance: While often assumed, it deserves constant measurement, especially in light of data format diversity.
6. Percentage of Fully Electronic Payments
Tracking what percent of payments are processed fully electronically (versus via checks or offline methods) is a great way to measure your digital transformation progress. Aim for at least 90%.
- High electronic rates ensure faster settlements, better auditability, and lower opportunities for errors or fraud.
- If your percentage is low, focus first on automating standard transaction types with reliable trading partners, gradually onboarding more complex or smaller ones.
Applying KPIs to EDI 834, 837, 999, and 277 Transactions
Let’s bring this into daily payer reality. Each EDI transaction type comes with unique KPI nuances and compliance requirements.
- EDI 834 (Enrollment): Track data loading latency, duplicate rate, data accuracy, and discrepancy acknowledgment time.
- EDI 837 (Claims): Focus on claim validation pass rates, time to adjudication, SNIP compliance, and first-pass resolution. Explore EDI KPIs in depth.
- EDI 999 (Acknowledgment): Prioritize speed of acknowledgment (ideally within 30 minutes), and completeness of returned error detail for rejected transactions. A reliable 999 process helps you recover and correct more quickly.
- EDI 277 (Claim Status): Key KPIs include accuracy of responses, response time, and closure rates for open inquiries. Timely and accurate 277s keep provider satisfaction high and reduce call center volumes.
Moving from Measurement to Improvement
Know your baseline for each metric, then track improvement quarter over quarter. A simple phased approach:
- Assess Your Current State: Gather 30-60 days’ data on error rates, touchless rate, days-to-pay, and SNIP compliance.
- Prioritize High-Impact Metrics: Start with those affecting revenue, compliance, or member/provider satisfaction.
- Implement Real-Time Dashboards: Stop relying on spreadsheets. Real-time dashboards let you spot and fix issues fast, enhancing team collaboration and accountability.
- Set Realistic Quarterly Targets: Strive for 10-20% annual improvement per key metric, adjusting as your automation journey matures.

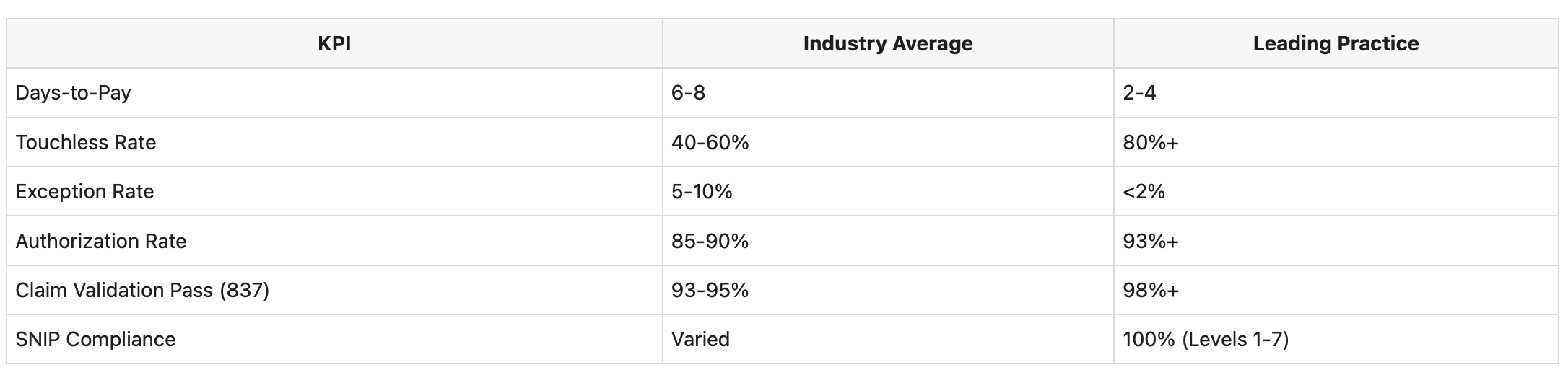
What Does Good Look Like? Sample Benchmarks
KPI Pitfalls to Avoid
- Tracking dozens of trivial KPIs instead of the few that matter most
- Setting unreasonable targets (like expecting 100% automation instantly)
- Measuring without timely review or ownership
- Failing to involve operations staff in interpretation and action
- Neglecting underlying data quality—your metrics are only as reliable as your data foundation
Maintain focus, review KPIs monthly, and empower teams to make adjustments based on data. When you act on these insights, you not only improve bottom-line results but also strengthen compliance and reduce operational headaches.
Bringing It All Together
As we push toward touchless, automated, and transparent processes across all enrollment and claim workflows, relentless measurement and continuous improvement are our best tools. Whether we're wrangling EDI 834 files from every imaginable source, adjudicating 837s in near real-time, or showing auditors a complete audit trail with every 999 and 277, the most effective teams make their metrics their guide every day.
If you’re ready to step into the upper quartile of efficiency and reliability, consider how integrated platforms and processes—like those we advocate at EDI Sumo—can help you reach and exceed your KPI goals. And for more practical strategies on bridging the gap between measurement and operational clarity, check out Solving the Next Layer of Healthcare Integration: Beyond EDI Pain Points to Enterprise Clarity.
When you're ready to take action or want to see how we can deliver real-time KPI visibility, automation, and auditability across your most critical healthcare transactions, connect with us at EDI Sumo.


.png)






.png)

.png)


.png)
