Demystifying EDI 277: Improving Claims Status Visibility for Health Insurance Payers

Electronic Data Interchange (EDI) is the lifeblood of efficient claims and enrollment processing for health insurance payers. Yet for many payer organizations, the details of certain EDI transactions—like the EDI 277 Claims Status Notification—remain unclear or even overwhelming. As a company that helps healthcare insurance providers untangle and standardize EDI processes, we at EDI Sumo have witnessed firsthand how proper 277 management improves claims workflow, streamlines customer service, and delivers greater enterprise-wide data visibility.
What is EDI 277? Why Does It Matter for Payers?
The EDI 277 transaction—formally called the Health Care Claim Status Notification—is an industry-standard document exchanged between health plans (payers), healthcare providers, and clearinghouses. It communicates the status of submitted medical, dental, or vision claims. Whether a claim is accepted, rejected, pending, or requires further information, payers rely on EDI 277 to keep everyone in the loop.
- Providers use the 277 to understand if their claims are being processed or need correction.
- Payers manage compliance, automate workflows, and identify errors early through robust 277 exchange.
- Members receive clearer guidance about their coverage and out-of-pocket costs.
The critical importance of 277 transactions goes beyond just regulatory compliance. Accurate, timely claim status updates help prevent payment delays, minimize denied claims, and improve both provider and member experiences—all of which have a direct impact on payer reputation and financial outcomes.
Decoding the Anatomy of EDI 277
Understanding what lives inside a 277 file is key for maximizing its utility.
- Status Segment: The heart of the 277—it contains the status code (e.g., accepted, rejected, pending) for each claim or service line.
- Claim Information: Details about each claim, including patient data, provider, and insurance identifiers.
- Error Reporting: If a claim is rejected or pended, specific error codes and sometimes narrative descriptions explain why.
- References/Correlations: Each status response includes tracking and control numbers that tie it back to the original claim (e.g., the EDI 837).
In practice, a single EDI 277 could report status for one claim or thousands—demanding robust systems for parsing, standardizing, and presenting these details for actionable insight.
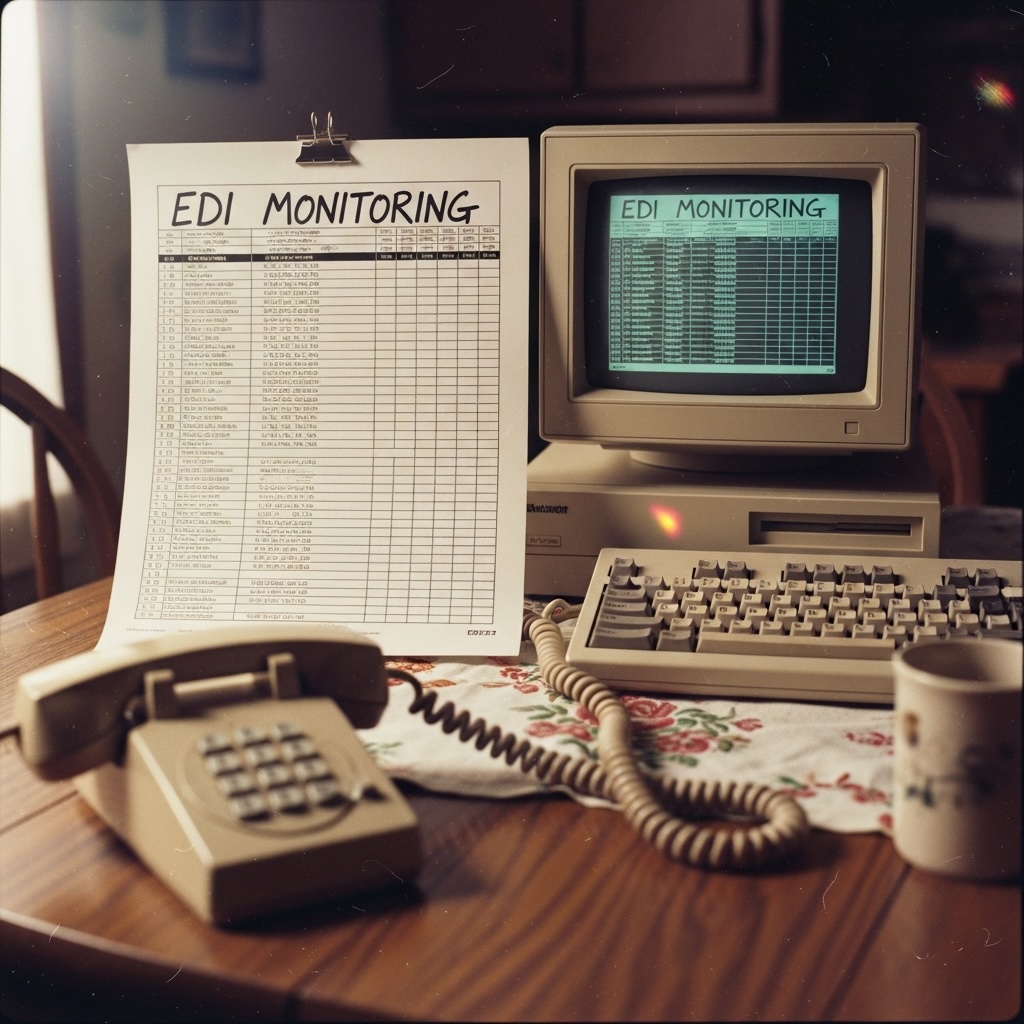
The EDI 277 Challenge: Fragmented Data, Siloed Systems
Despite the potential, many payer organizations still handle EDI 277 transactions as a technical afterthought. What are the real-world problems we hear?
- Siloed claim status details locked in legacy EDI translators or clearinghouse portals
- Manual “swivel chair” efforts by customer service to look up claim status
- Difficulty linking 277 updates to the original claim, especially when formats and trading partner conventions vary
- Operational delays from error-prone manual mapping or ad-hoc spreadsheet workarounds
- Compliance risks and audit anxiety due to lack of real-time traceability and audit trails
The result? Frustration for support staff, longer provider and member wait times, unnecessary downstream claim pends or denials, and heightened risk of missed SLAs and compliance issues.
How EDI Sumo Clears the Fog: From 277 Chaos to Claims Status Clarity
At EDI Sumo, we've built our platform and services specifically for health insurance payers who want to modernize their EDI lifecycle—without adding burden to busy IT teams or having to overhaul mission-critical claims systems. Here’s how our approach unlocks the true power of EDI 277:
1. Multi-Format Standardization for All EDI Transactions
No matter the 277 variant—whether it’s EDI X12, positional files, XML, CSV, or other formats—our platform ingests and normalizes every claim status update. This means:
- No more tedious manual mapping for each trading partner or file format
- Immediate, standardized access to claim status across your entire enterprise
2. Real-Time Monitoring and Error Detection
Track every 277 transaction as soon as it arrives. Automated error detection and discrepancy alerts notify teams instantly when a claim is rejected, pended, or requires additional information—minimizing payment delays and preventing backlogs.
3. Seamless Integration and Role-Based Access
We understand not every payer can (or should) rip and replace existing claims adjudication systems and EDI translators. EDI Sumo sits atop your current stack, bringing next-generation EDI management capabilities:
- Unified dashboards for claims, eligibility, and status, available in real-time
- Role-based access so the right information is instantly available to support agents, enrollment managers, and compliance teams
- Automated audit trails for every claims status interaction
4. Actionable Reporting & SLA Assurance
We take the guesswork out of regulatory compliance and SLA monitoring:
- Custom reporting modules that surface trends in rejected or slow-moving claims
- Performance dashboards to monitor SLA adherence end to end
- Exportable audit logs for trading partner reviews and regulatory audits
5. HIPAA Compliance, Out of the Box
Security and privacy aren’t optional. EDI Sumo is built to meet HIPAA, GDPR, and related mandates, ensuring data is appropriately encrypted, access-controlled, and always audit-ready.

Unlocking Value for Every Stakeholder
When handled right, EDI 277 data becomes much more than a regulatory hoop to jump through. Here’s how it serves every corner of your payer organization:
- IT and EDI Operators: Eliminate manual workarounds and repetitive queries by automating, normalizing, and centralizing 277 management.
- Customer Support: Instantly surface claim status for every member or provider call, resolving issues in minutes—not days.
- Compliance and Audit: Enjoy real-time, detailed audit trails for every 277 touchpoint—ready for trading partner and regulatory review.
- Operations and Management: Visualize bottlenecks, quickly identify trends in pended or denied claims, and optimize your claims workflow end to end.
Best Practices: Elevating Claims Status Visibility
Whether you leverage EDI Sumo or another solution, these are best practices we've seen elevate payer performance with 277 management:
- Automate Ingestion and Parsing: Manual review of 277 files is unsustainable at scale. Use robust automation to standardize, validate, and extract claim status details as soon as updates arrive.
- Centralized, Real-Time Access: Make claim status visible to all relevant roles through a unified dashboard—no more chasing emails or hopping systems.
- Tie 277s to Original Claims: Ensure every status is tied back to its originating EDI 837 (or other claim document) for a 360-degree view of each transaction.
- Audit and Report Proactively: Use customizable dashboards and automated logs for SLA, compliance, and operational reporting—before auditors or trading partners ask.
- Integrate with Customer Service: Empower your support teams to resolve complex provider or member inquiries with instantaneous, accurate claim status details and history.
The Road Ahead: Turning Data Into Action
If your health plan is still managing EDI 277 files in isolation or with a mountain of spreadsheets, the door is open for significant efficiency and service gains. With the volume and complexity of EDI only increasing—especially as payers and providers demand transparency and faster claim resolution—the ability to transform raw status notifications into actionable, accessible intelligence will become a key competitive advantage.

Why Partner with EDI Sumo for EDI 277 Mastery?
At EDI Sumo, we’ve dedicated ourselves to eliminating the friction and guesswork of healthcare EDI, including the nuances of 277 status notifications. Our platform helps payers:
- Handle EDI 277 in all major formats, standardizing data for the enterprise
- Gain real-time, actionable visibility for claims and enrollment status
- Automate compliance, monitoring, and error response—reducing SLA penalties and freeing vital IT resources
- Refocus support teams and management on member and provider service, not manual data wrangling
If you’re ready to move beyond EDI status quo and want to empower every team member with the data and tools they deserve, reach out to us at EDI Sumo. Schedule a personalized demo and see firsthand how we can help your organization make claims status visibility a true business asset—not a technical challenge.


.png)




.png)

.png)


.png)
