Building Event-Driven EDI: Streaming Alerts and Replays That Keep Operations in Sync

Healthcare payers today are juggling a complex mix of enrollment formats, regulatory requirements, and ever-increasing expectations for data accuracy and timeliness. Traditional batch-driven EDI models create delays and information silos that can lead to costly errors, SLA breaches, and mounting frustration for everyone from IT directors to customer service teams. We believe the shift to event-driven EDI is imperative for payers who want real-time clarity and true operational sync across the enterprise.
Understanding the Shift: What Makes Event-Driven EDI Stand Out?
Traditional batch EDI models are set around fixed processing windows. Files are dropped at specific times (often overnight), processed in bulk, and only later are errors surfaced to your teams. This delay makes it difficult to address discrepancies before they ripple out to claims, member experiences, or compliance obligations.
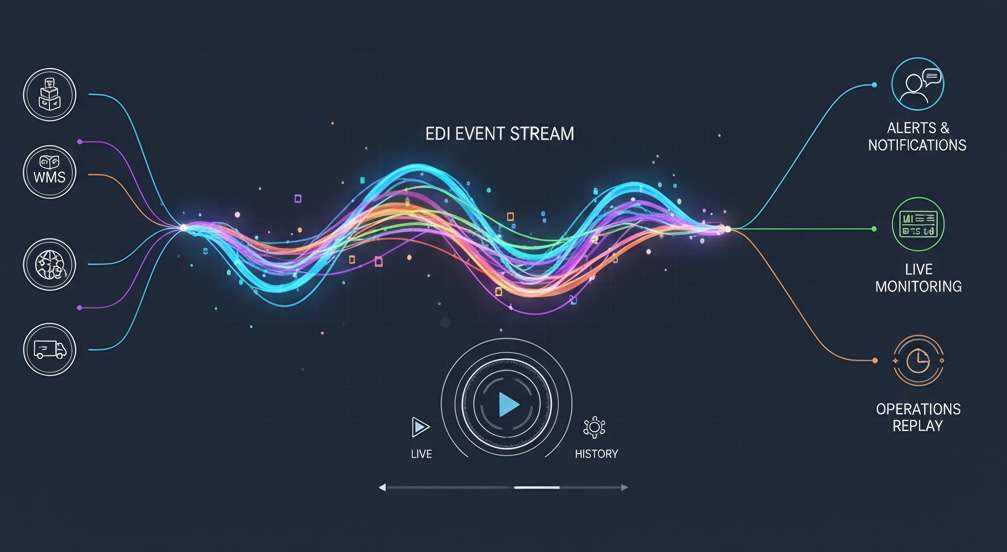
With event-driven EDI, every update—such as a new enrollment file, an eligibility change, or a claim submission—becomes an actionable event. The system generates real-time notifications, automatically triggers resolutions, and keeps a detailed audit trail. Your teams are empowered to act as soon as issues surface, instead of playing catch-up after problems have already spread across your workflows. This means fewer delays, reduced manual intervention, and significant improvements in data quality and operations.
Core Building Blocks: How Event-Driven EDI Works
- Event Producers: These are the sources of new data in your ecosystem, including trading partners, providers, and internal processes. Each data change triggers an event, whether it is an EDI 834 enrollment file, a CSV upload, or an XML claim submission. It is crucial these diverse inputs are standardized for downstream use. At EDI Sumo, we ingest EDI, positional, CSV, and XML formats then transform them for unified event processing.
- Event Routers: These systems receive and intelligently distribute events based on business rules. For example, a record with an eligibility conflict might route to compliance for review, while a high-value claim might go straight to fraud prevention. By routing information only where it matters, we help teams focus on what is truly important without being overwhelmed by irrelevant alerts.
- Event Consumers: These are systems and teams that take action including claims management, customer service reps, analytics dashboards, and compliance monitors. They each subscribe to the types of events that match their role. A single enrollment event can update your eligibility system, alert a customer service agent, and log a compliance trace, all in parallel, eliminating the bottlenecks of serial batch jobs.
Streaming Alerts: Keeping Teams Informed and Proactive
Streaming alerts in an event-driven system are a game changer for payer operations. You get:
- Validation Alerts: Instantly flag issues like missing or invalid data—whether it’s a subscriber ID or provider NPI—so your team can address them before they impact downstream processing.
- Performance Alerts: Let you know when processing speeds deviate from the norm, flagging potential infrastructure or connectivity issues in real time.
- Compliance Alerts: Notify users proactively if SLAs are at risk or when data access patterns are unusual, supporting HIPAA and internal policy adherence.
We make sure that these alerts are routed based on both context and priority. Non-critical errors may go to the EDI coordinator for review, while urgent system outages are escalated to IT leadership. By assigning alerts intelligently, we help reduce alert fatigue and make sure the right person sees the right information at the right time.
Replay Capabilities: Reducing Data Loss and Downtime
Even with real-time monitoring, no system is immune to outages, network glitches, or partner issues. This is where replay capabilities in event-driven EDI make the difference.
- Every transaction and event is logged with sequence and metadata. If a downstream system is offline—say, during a patch or unexpected downtime—events are stored safely and replayed once normal operations resume.
- This approach means fewer manual recovery processes, and it guards against data loss. If claims or enrollments arrive during maintenance, once your systems are restored, all missed events are processed in order, ensuring your audit trail is complete and compliant with regulations like HIPAA.
- Replay also simplifies corrections. If a trading partner submits faulty data, you can replay just the corrected events and have all connected systems update in sync.
Keeping Your Ecosystem in Sync Across All Formats
Healthcare payers work with various systems: enrollment and eligibility databases, claims engines, customer support desks, and analytics tools. Historically, synchronizing these required periodic batch updates and multiple reconciliation jobs, often leaving teams with outdated or conflicting data. Event-driven EDI removes this lag by letting every system receive updates from the same underlying stream of events.
- When an eligibility change happens, it is instantly reflected in all connected systems.
- Your analytics dashboard displays real-time numbers, not yesterday’s figures.
- Customer service teams always have the latest member data at their fingertips, reducing call escalations and improving member satisfaction.
One of our biggest challenges is integrating across diverse partner formats. By normalizing EDI, Excel, CSV, positional, and XML inputs, we maintain operational clarity regardless of the format or delivery method a partner chooses. This single-source-of-truth architecture is critical for reducing operational headaches and keeping every system accurate and consistent.

Actionable Steps: Moving to Event-Driven EDI
- Assemble Your Implementation Team
Engage leaders from IT, EDI, enrollments, claims, and compliance. Assign a project sponsor with authority to support cross-department initiatives. - Audit and Map Existing Processes
Document every step of your enrollment, claims, trading partner management, and support workflows. Identify where delays, manual touchpoints, and recurring issues occur. - Define Alert Taxonomies and Routing
Decide which events require alerts, who should receive them, and at what severity level. Be clear about thresholds, escalation paths, and response protocols. - Design Your Event Schema
Choose standardized structures for enrollment, claims, and error events. This assures all systems can subscribe to and understand the events being pushed. - Select Technology With Multi-Format Support
Your solution should natively handle EDI, CSV, XML, and positional files. Automated alerts, custom validations, and seamless integration options are essential. - Start With a High-Impact Pilot
Enrollment processes are usually high volume and time sensitive, making them ideal for piloting event-driven EDI. Run both event and batch workflows in parallel to validate the new approach and build stakeholder confidence. - Expand Gradually
Once your pilot succeeds, roll out to additional workflows and trading partners, ensuring each step is fully validated and operationally sound.
Practical Benefits You Can Expect
- Faster Response Times: Errors surface within minutes. EDI coordinators and support staff can address problems the same day, not the next morning.
- Higher Data Accuracy: Proactive validation stops errors from reaching claims engines or billing systems, reducing rework and member complaints.
- Greater Reliability: Replay eliminates manual data recovery and reduces downtime during system maintenance.
- Simplified Compliance: Continuous audit trails make it easier to prove HIPAA compliance to internal and external auditors.
We have seen organizations shrink discovery windows for enrollment issues from hours to a few minutes. Alert fatigue is reduced due to smarter routing, and overall system resilience improves since outages no longer mean missing or duplicating files.
Frequently Asked Questions About Event-Driven EDI
- Will real-time alerts overwhelm my team? When designed right, alert routing keeps noise low and focuses attention on real, actionable issues.
- Is a full platform replacement required? Not usually. Event-driven models wrap around existing eligibility, claims, and partner platforms, transforming only how data flows and is monitored.
- Can we support partners using old batch methods? Absolutely. We treat file arrivals, API calls, and even SFTP uploads as events for internal handling, regardless of how a partner chooses to deliver data.
Planning Your Event-Driven EDI Roadmap
Our approach is built on making data unified, instantly actionable, and traceable from the moment it enters your domain to every point it is consumed or reported. This level of clarity helps payers not only meet but exceed member expectations for speed, accuracy, and responsiveness.
Adopting event-driven EDI starts with evaluating your current state and mapping where real-time sync and streaming alerts could drive the most value. If you are considering this transformation, we are here to help. Explore what is possible or schedule a discovery session at EDI Sumo.


.png)






.png)

.png)


.png)
